Theme: Therapeutic Approaches for Diabetes Management and Endocrine Complications
Diabetes Asia Pacific 2018
Being perceived as an incredibly Reputed Organization, Conference Series invites the worldwide global audience and presenters to participate at the 20th Asia Pacific Diabetes Conference which is to be held in Sydney, Australia during July 16-17, 2018. Special interest and theme of the conference is “Therapeutic Approaches for Diabetes Management and endocrine complications”.
Diabetes is a disease that affects your body's ability to produce or use insulin. Insulin is a hormone. When your body turns the food you eat into energy (also called sugar or glucose), insulin is released to help transport this energy to the cells. Insulin acts as a “key.” Diabetes, often referred to by doctors as diabetes mellitus, describes a group of metabolic diseases in which the person has high blood glucose (blood sugar), either because insulin production is inadequate, or because the body's cells do not respond properly to insulin, or both.
Diabetes Asia Pacific 2018 is an international platform for presenting research about diabetes management and therapeutics, exchanging ideas about it and thus, contributes to the dissemination of knowledge in management of the disease for the benefit of the society. Diabetes Asia Pacific 2018 is where the future of management and novel therapeutics for the disease intersects.
The Annual conference aims to provide an opportunity to share knowledge, expertise along with unparalleled networking opportunities between a large number of medical and industrial professionals in this sphere. The meeting gathers renowned scientists, physicians, surgeons, young researchers, industrial delegates and talented student communities in the field of diabetic medicine under a single roof where networking and global partnering happens for the acceleration of future research.
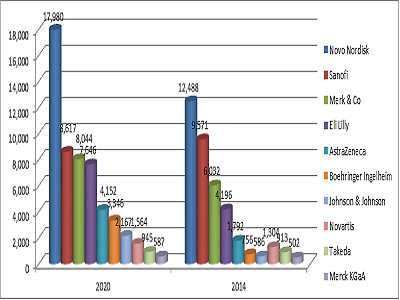
The drugs market in field of internal Medicine especially in diabetes and Endocrinology in America is expected to reach USD 41 billion by 2020, growing at a CAGR of over 6%.The drugs market in EMEA will exceed USD 16 billion by 2020, growing at a CAGR of over 6%. The drugs market in APAC is expected to exceed USD 14 billion by 2020, growing at a CAGR of over 7%. Key suppliers are Novo Nordisk, Sanofi, Merck, Eli Lilly, AstraZeneca, and AbbVie
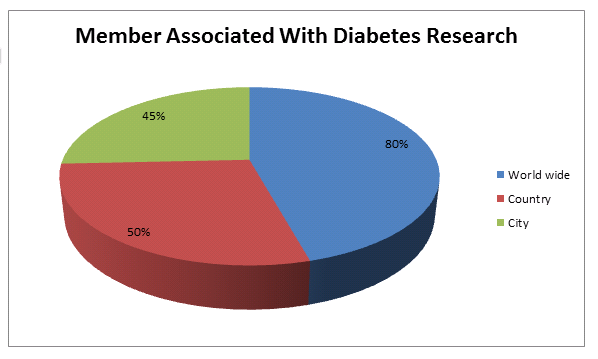
Conference Series Ltd organizes a conference series of 1000+ Global Events inclusive of 300+ Conferences, 500+ Upcoming and Previous Symposiums and Workshops in USA, Europe & Asia with support from 1000 more scientific societies and publishes 700+ Open access journals which contains over 30000 eminent personalities, reputed scientists as editorial board members
Why to attend?
Diabetes Asia Pacific 2018 highlights the theme “Therapeutic Approaches for Diabetes Management and endocrine complications” Which emphasis on the latest advancements in prevention and treatment cure of various metabolic diseases which may be due to diabetic and endocrine complications and provides robust discussions on methods and strategies related to diagnosis, prevention and management of metabolic disorders as well as explore new ideas and concepts for treatment of Endocrine Complications..
Target Audience:
- Endocrinologists
- Diabetologists
- Researchers
- Practitioners/Doctors
- Students
- Nurse educator
- Podiatrist
- Dietitian
- Eye Doctors
- Nephrologists
- Physical trainer or Exercise physiologist
Track 1 : Pre-Diabetes/Borderline Diabetes (Pre-cursor to Diabetes Mellitus):
Prediabetes, also commonly referred to as borderline diabetes, is a metabolic condition and growing global problem that is closely tied to obesity. Prediabetes is the precursor stage before diabetes mellitus in which not all of the symptoms required to diagnose diabetes are present, but blood sugar is abnormally high. Prediabetes is characterized by the presence of blood glucose levels that are higher than normal but not yet high enough to be classed as diabetes.
For this reason, prediabetes is often described as the “gray area” between normal blood sugar and diabetic levels. In the UK, around 7 million people are estimated to have prediabetes and thus have a high risk for developing type 2 diabetes. Prediabetes is associated with obesity (especially abdominal or visceral obesity), dyslipidemia with high triglycerides and/or low HDL cholesterol, and hypertension. It is thus a metabolic diathesis or syndrome, and it usually involves no symptoms and only high blood sugar as the sole sign.
The progression to type 2 diabetes mellitus is not inevitable for those with prediabetes. The progression into diabetes mellitus from prediabetes is approximately 25% over three to five years. For patients with severe risk factors, prescription medication may be appropriate. This may be considered in patients for whom lifestyle therapy has failed, or is not sustainable, and who are at high-risk for developing type 2 diabetes. Metformin and acarbose help prevent the development of frank diabetes, and also have a good safety profile. The most serious consequence of prediabetes is progression to type 2 diabetes.
Related Conferences: 22nd International Congress on Prevention of Diabetes and Complications October 12-13, 2017 London, UK; 9th Annual Congress on Endocrine Disorders and Therapies October 30- November 1, 2017; 23rd International Conference on Herbal and Alternative Remedies for Diabetes and Endocrine Disorders November 2-4, 2017 Bangkok, Thailand; 25th Global Diabetes Summit and Medicare Expo December 04-05, 2017 Dubai, UAE; 10th International Conference on Endocrinology October 30-November 01, 2017 Chicago, Illinois, USA; 17th Global Diabetes Conference and Medicare Expo March 8-9, 2018 Paris, France; 27th European Diabetes Congress June 11-12, 2018 Rome, Italy; 20th Asia Pacific Diabetes Conference July 16-17, 2018 Sydney, Australia; International Conference on Diabetes and its Complications May 21-22,2018 Osaka, Japan
Track 2 :Influence of genetics on Diabetes:
Several gene mutations have been linked to the development of type 2 diabetes. These gene mutations can interact with the environment and each other to further increase your risk. Type 2 diabetes is caused by both genetic and environmental factors.
Scientists have linked several gene mutations to a higher diabetes risk. Not everyone who carries a mutation will get diabetes. But many people with diabetes do have one or more of these mutations.
It can be difficult to separate genetic risk from environmental risk. The latter is often influenced by your family members. For example, parents with healthy eating habits are likely to pass them on to the next generation. On the other hand, genetics plays a big part in determining weight.
Mutations in any gene involved in controlling glucose levels can increase your risk of type 2 diabetes.
Related Conferences: 23rd International Conference on Herbal and Alternative Remedies for Diabetes and Endocrine Disorders November 2-4, 2017 Bangkok, Thailand; 25th Global Diabetes Summit and Medicare Expo December 04-05, 2017 Dubai, UAE; 10th International Conference on Endocrinology October 30-November 01, 2017 Chicago, Illinois, USA; 17th Global Diabetes Conference and Medicare Expo March 8-9, 2018 Paris, France; 27th European Diabetes Congress June 11-12, 2018 Rome, Italy; 20th Asia Pacific Diabetes Conference July 16-17, 2018 Sydney, Australia; International Conference on Diabetes and its Complications May 21-22,2018 Osaka, Japan;22nd International Congress on Prevention of Diabetes and Complications October 12-13, 2017 London, UK; 9th Annual Congress on Endocrine Disorders and Therapies October 30- November 1, 2017;
Track 3 :Metabolic Syndrome/Syndrome X:
Metabolic syndrome is a cluster of conditions — increased blood pressure, high blood sugar, excess body fat around the waist, and abnormal cholesterol or triglyceride levels — that occur together, increasing your risk of heart disease, stroke and diabetes. Metabolic syndrome is closely linked to overweight or obesity and inactivity.
It's also linked to a condition called insulin resistance. Normally, your digestive system breaks down the foods you eat into sugar (glucose). Insulin is a hormone made by your pancreas that helps sugar enter your cells to be used as fuel.
In people with insulin resistance, cells don't respond normally to insulin, and glucose can't enter the cells as easily. As a result, glucose levels in your blood rise despite your body's attempt to control the glucose by churning out more and more insulin.
Related Conferences: 20th Asia Pacific Diabetes Conference July 16-17, 2018 Sydney, Australia; International Conference on Diabetes and its Complications May 21-22,2018 Osaka, Japan; 22nd International Congress on Prevention of Diabetes and Complications October 12-13, 2017 London, UK; 9th Annual Congress on Endocrine Disorders and Therapies October 30- November 1, 2017; 23rd International Conference on Herbal and Alternative Remedies for Diabetes and Endocrine Disorders November 2-4, 2017 Bangkok, Thailand; 25th Global Diabetes Summit and Medicare Expo December 04-05, 2017 Dubai, UAE; 27th European Diabetes Congress June 11-12, 2018 Rome, Italy.
Track 4: Insulin- Important Pancreatic hormone:
Insulin is a hormone made by the pancreas that allows your body to use sugar (glucose) from carbohydrates in the food that you eat for energy or to store glucose for future use. Insulin helps keeps your blood sugar level from getting too high (hyperglycemia) or too low (hypoglycemia).
The cells in your body need sugar for energy. However, sugar cannot go into most of your cells directly. After you eat food and your blood sugar level rises, cells in your pancreas (known as beta cells) are signaled to release insulin into your bloodstream. Insulin then attaches to and signals cells to absorb sugar from the bloodstream. Insulin is often described as a “key,” which unlocks the cell to allow sugar to enter the cell and be used for energy.
Insulin can be given by a syringe, injection pen, or an insulin pump that delivers a continuous flow of insulin. The purpose of the Patient Guide to Insulin is to educate patients, parents, and caregivers about insulin treatment of diabetes.
Related Conferences: 25th Global Diabetes Summit and Medicare Expo December 04-05, 2017 Dubai, UAE; 27th European Diabetes Congress June 11-12, 2018 Rome, Italy; 20th Asia Pacific Diabetes Conference July 16-17, 2018 Sydney, Australia; International Conference on Diabetes and its Complications May 21-22,2018 Osaka, Japan; 22nd International Congress on Prevention of Diabetes and Complications October 12-13, 2017 London, UK; 9th Annual Congress on Endocrine Disorders and Therapies October 30- November 1, 2017; 23rd International Conference on Herbal and Alternative Remedies for Diabetes and Endocrine Disorders November 2-4, 2017 Bangkok, Thailand;
Track 5: Diabetic Kidney Disease (Diabetic Nephropathy):
Diabetes causes injury to small blood vessels in the body.
When the blood vessels in the kidneys are injured, your kidneys cannot clean your blood properly. Your body will retain more water and salt than it should, which can result in weight gain and ankle swelling. You may have protein in your urine. Also, waste materials will build up in your blood.
Diabetes also may cause damage to nerves in your body. This can cause difficulty in emptying your bladder. The pressure resulting from your full bladder can back up and injure the kidneys. Also, if urine remains in your bladder for a long time, you can develop an infection from the rapid growth of bacteria in urine that has a high sugar level.
About 30 percent of patients with Type 1 (juvenile onset) diabetes and 10 to 40 percent of those with Type 2 (adult onset) diabetes eventually will suffer from kidney failure.
The earliest sign of diabetic kidney disease is an increased excretion of albumin in the urine.
Related Conferences: 20th Asia Pacific Diabetes Conference July 16-17, 2018 Sydney, Australia; International Conference on Diabetes and its Complications May 21-22,2018 Osaka, Japan; 25th Global Diabetes Summit and Medicare Expo December 04-05, 2017 Dubai, UAE; 27th European Diabetes Congress June 11-12, 2018 Rome, Italy; 22nd International Congress on Prevention of Diabetes and Complications October 12-13, 2017 London, UK; 9th Annual Congress on Endocrine Disorders and Therapies October 30- November 1, 2017; 23rd International Conference on Herbal and Alternative Remedies for Diabetes and Endocrine Disorders November 2-4, 2017 Bangkok, Thailand;
Track 6: Diabetic Eye Disease(Diabetic Retinopathy):
Diabetic retinopathy is caused by changes in the blood vessels of the retina, the thin, light-sensitive inner lining in the back of your eye. This damage, called retinopathy, occurs to small blood vessels in the retina, which are easily harmed by high levels of glucose in the blood. There are two stages of diabetic retinopathy—an initial stage, which is called nonproliferative retinopathy, and a more serious stage called proliferative retinopathy, in which there is a greater risk of hemorrhage into the vitreous or detachment of the retina leading to severe vision loss. Another condition, called diabetic macular edema, can occur with either stage.
Related Conferences: 20th Asia Pacific Diabetes Conference July 16-17, 2018 Sydney, Australia; International Conference on Diabetes and its Complications May 21-22,2018 Osaka, Japan; 25th Global Diabetes Summit and Medicare Expo December 04-05, 2017 Dubai, UAE; 27th European Diabetes Congress June 11-12, 2018 Rome, Italy; 22nd International Congress on Prevention of Diabetes and Complications October 12-13, 2017 London, UK; 9th Annual Congress on Endocrine Disorders and Therapies October 30- November 1, 2017; 23rd International Conference on Herbal and Alternative Remedies for Diabetes and Endocrine Disorders November 2-4, 2017 Bangkok, Thailand;
Track 7 :Complications of Diabetes:
Uncontrolled diabetes can lead to a number of short and long-term health complications, including hypoglycemia, heart disease, nerve damage and amputation, and vision problems. The majority of these diabetes-related conditions occur as a result of uncontrolled blood glucose levels, particularly elevated blood sugar over a prolonged period of time. It is common for most people with diabetes to begin to develop complications after having diabetes for a number of years.
With good diabetes control and living a healthy, active lifestyle, it is possible for people to go a number of decades complication free. The long-term measure of blood glucose is important for people with diabetes as the higher their HbA1c value, the greater the risk of developing serious diabetic complications.
By reducing HbA1c and keeping blood pressure and cholesterol levels well controlled, people with diabetes can reduce their risk of diabetic complications.
Related Conferences: 25th Global Diabetes Summit and Medicare Expo December 04-05, 2017 Dubai, UAE; 27th European Diabetes Congress June 11-12, 2018 Rome, Italy; 22nd International Congress on Prevention of Diabetes and Complications October 12-13, 2017 London, UK; 9th Annual Congress on Endocrine Disorders and Therapies October 30- November 1, 2017; 23rd International Conference on Herbal and Alternative Remedies for Diabetes and Endocrine Disorders November 2-4, 2017 Bangkok, Thailand; 20th Asia Pacific Diabetes Conference July 16-17, 2018 Sydney, Australia; International Conference on Diabetes and its Complications May 21-22,2018 Osaka, Japan
Track 8: Diabetic Transplantations:
Type 1 diabetes results from the destruction of insulin-producing cells in the islets of the pancreas. Islet cell transplantation involves extracting islet cells from the pancreas of a deceased donor and implanting them in the liver of someone with Type 1. This minor procedure is usually done twice for each transplant patient, and can be performed with minimal risk using a needle under local anaesthetic. Islet transplants have been shown to reduce the risk of severe hypos. Results from UK islet transplant patients showed that the frequency of hypos was reduced from 23 per person per year before transplantation to less than one hypo per person per year afterwards.
Islet transplants usually also lead to improved awareness of hypoglycaemia, less variability in blood glucose levels, improved average blood glucose, improved quality of life and reduced fear of hypos. Long-term results are good and are improving all the time. For example, the majority of transplant patients can now expect to have a functioning transplant after six years and some people have had more than 10 years of clinical benefit.
Related Conferences: 23rd International Conference on Herbal and Alternative Remedies for Diabetes and Endocrine Disorders November 2-4, 2017 Bangkok, Thailand; 20th Asia Pacific Diabetes Conference July 16-17, 2018 Sydney, Australia; International Conference on Diabetes and its Complications May 21-22,2018 Osaka, Japan; 25th Global Diabetes Summit and Medicare Expo December 04-05, 2017 Dubai, UAE; 27th European Diabetes Congress June 11-12, 2018 Rome, Italy; 22nd International Congress on Prevention of Diabetes and Complications October 12-13, 2017 London, UK; 9th Annual Congress on Endocrine Disorders and Therapies October 30- November 1, 2017;
Track 9: Important Tests to Diagnose Diabetes:
Symptoms of severe increased thirst, frequent urination, unexplained weight loss, increased hunger, tingling of your hands or feet indicates to run a test for diabetes.
To confirm the diagnosis of type 2 diabetes, your doctor will order a fasting plasma glucose test or casual plasma glucose. The fasting plasma glucose test (FPG) is the preferred method for diagnosing diabetes, because it is easy to do, convenient, and less expensive than other tests. Before taking the blood glucose test, you will not be allowed to eat anything for at least eight hours. During a blood glucose test, blood will be drawn and sent to a lab for analysis.
Normal fasting blood glucose -- or blood sugar -- is between 70 and 100 milligrams per deciliter or mg/dL for people who do not have diabetes. The standard diagnosis of diabetes is made when two separate blood tests show that your fasting blood glucose level is greater than or equal to 126 mg/dL.
The casual plasma glucose test is another method of diagnosing diabetes. During the test, blood sugar is tested without regard to the time since the person's last meal. You are not required to abstain from eating prior to the test.
A glucose level greater than 200 mg/dL may indicate diabetes, especially if the test is repeated at a later time and shows similar results.
The hemoglobin A1c test (also called the glycated hemoglobin test or HbA1c), is an important diabetes blood test used to determine how well your diabetes is being controlled. Early detection of eye and foot problems in diabetes allows your doctor to prescribe proper treatment when it is most effective.
Related Conferences: 20th Asia Pacific Diabetes Conference July 16-17, 2018 Sydney, Australia; International Conference on Diabetes and its Complications May 21-22,2018 Osaka, Japan; 25th Global Diabetes Summit and Medicare Expo December 04-05, 2017 Dubai, UAE;23rd International Conference on Herbal and Alternative Remedies for Diabetes and Endocrine Disorders November 2-4, 2017 Bangkok, Thailand; 27th European Diabetes Congress June 11-12, 2018 Rome, Italy; 22nd International Congress on Prevention of Diabetes and Complications October 12-13, 2017 London, UK; 9th Annual Congress on Endocrine Disorders and Therapies October 30- November 1, 2017;
Track 10: Management of Diabetes:
The main goal of diabetes management is, as far as possible, to restore carbohydrate metabolism to a normal state. To achieve this goal, individuals with an absolute deficiency of insulin require insulin replacement therapy, which is given through injections or an insulin pump. Insulin resistance, in contrast, can be corrected by dietary modifications and exercise. Other goals of diabetes management are to prevent or treat the many complications that can result from the disease itself and from its treatment.
Modification of adverse lifestyle factors is an important aspect of the management of all types of diabetes. In particular, appropriate management of cardiovascular risk factors such as smoking, physical inactivity and poor diet is important for the prevention of macrovascular disease. Microvascular complications may also be affected by adverse lifestyle factors, eg smoking. However, helping patients to modify certain behaviors should take account of other factors such as the patient’s willingness to change, their perception of their diabetes, and factors which may be indirectly related to their diabetes, such as depression and adverse effects on quality of life.
Related Conferences: 20th Asia Pacific Diabetes Conference July 16-17, 2018 Sydney, Australia; International Conference on Diabetes and its Complications May 21-22,2018 Osaka, Japan; 25th Global Diabetes Summit and Medicare Expo December 04-05, 2017 Dubai, UAE;23rd International Conference on Herbal and Alternative Remedies for Diabetes and Endocrine Disorders November 2-4, 2017 Bangkok, Thailand; 27th European Diabetes Congress June 11-12, 2018 Rome, Italy; 22nd International Congress on Prevention of Diabetes and Complications October 12-13, 2017 London, UK; 9th Annual Congress on Endocrine Disorders and Therapies October 30- November 1, 2017;
Track 11:Diabetes Oral Medications/Anti-Diabetic Medications:
Drugs used in diabetes treat diabetes mellitus by lowering glucose levels in the blood. With the exceptions of Insulin, exenatide, liraglutide and pramlintide, all are administered orally and are thus also called oral hypoglycemic agents or oral antihyperglycemic agents. There are different classes of anti-diabetic drugs, and their selection depends on the nature of the diabetes, age and situation of the person, as well as other factors.
Diabetes mellitus type 1 is a disease caused by the lack of insulin. Insulin must be used in Type I, which must be injected.
Diabetes mellitus type 2 is a disease of insulin resistance by cells. Type 2 diabetes mellitus is the most common type of diabetes. Treatments include (1) agents that increase the amount of insulin secreted by the pancreas, (2) agents that increase the sensitivity of target organs to insulin, and (3) agents that decrease the rate at which glucose is absorbed from the gastrointestinal tract.
Several groups of drugs, mostly given by mouth, are effective in Type II, often in combination. Insulin sensitizers address the core problem in Type II diabetes—insulin resistance.
Thiazolidinediones (TZDs), also known as "glitazones," bind to PPARγ, a type of nuclear regulatory protein involved in transcription of genes regulating glucose and fat metabolism.
Secretagogues are drugs that increase insulin output from the pancreas. Meglitinides help the pancreas produce insulin and are often called "short-acting secretagogues".
Alpha-glucosidase inhibitors are "diabetes pills" but not technically hypoglycemic agents because they do not have a direct effect on insulin secretion or sensitivity. Dipeptidyl peptidase-4 (DPP-4) inhibitors increase blood concentration of the incretin GLP-1 by inhibiting its degradation by dipeptidyl peptidase-4.
Related Conferences: 20th Asia Pacific Diabetes Conference July 16-17, 2018 Sydney, Australia; International Conference on Diabetes and its Complications May 21-22,2018 Osaka, Japan; 25th Global Diabetes Summit and Medicare Expo December 04-05, 2017 Dubai, UAE;23rd International Conference on Herbal and Alternative Remedies for Diabetes and Endocrine Disorders November 2-4, 2017 Bangkok, Thailand; 27th European Diabetes Congress June 11-12, 2018 Rome, Italy; 22nd International Congress on Prevention of Diabetes and Complications October 12-13, 2017 London, UK; 9th Annual Congress on Endocrine Disorders and Therapies October 30- November 1, 2017;
Track 12: Approaches and technologies for the Treatment of Diabetes:
The concept of 'new technologies' for type 1 diabetes and new discovery and advanced type 2 diabetes treatment has expanded in recent years at a rate that some might consider comparable to 'Moore’s Law', and the sheer number of new technologies entering into the type 1 diabetes marketplace is also growing at a remarkable rate. From the patient’s perspective, this is not only exciting but can lead to a sense of optimism. Technologies that today are growing commonplace (e.g. insulin pumps, rapid HbA1c monitoring, etc. come under new therapeutic mechanisms of diabetes. Indeed, it could be argued that the major advances in type 1 diabetes care made within the last quarter of a century have come from technology rather than biology. At the same time, not all new technologies succeed (e.g. the Glucowatch), regardless of their purported promise. Both type 1 diabetes patients and their healthcare providers will soon see a series of further advanced medical technologies used in hospital and new technologies and novel therapies in diabetes treatment whose basis is tied to the notion of improving the lives of those with the disease.
The aim of diabetes treatment is to keep, within reason, blood glucose levels as near to normal as possible. Training in self-management of diabetes forms an essential part of diabetes management. Treatment should be agreed on an individual basis and address medical, psychosocial and lifestyle issues.
A variety of different factors have a role to play in treating diabetes, but the importance of balanced, co-ordinated diabetes treatment for all diabetics cannot be underestimated.
Regular and successful treatment decreases the risk of each patient developing diabetes complications.
Related Conferences: 20th Asia Pacific Diabetes Conference July 16-17, 2018 Sydney, Australia; International Conference on Diabetes and its Complications May 21-22,2018 Osaka, Japan; 25th Global Diabetes Summit and Medicare Expo December 04-05, 2017 Dubai, UAE;23rd International Conference on Herbal and Alternative Remedies for Diabetes and Endocrine Disorders November 2-4, 2017 Bangkok, Thailand; 27th European Diabetes Congress June 11-12, 2018 Rome, Italy; 22nd International Congress on Prevention of Diabetes and Complications October 12-13, 2017 London, UK; 9th Annual Congress on Endocrine Disorders and Therapies October 30- November 1, 2017;
Track 13: New Diabetes Treatments-Boost to blood flow:
Three diabetes treatments with entirely new modes of action were approved: exenatide injection for people with type 2 diabetes, pramlintide injection as an add-on to insulin therapy for people with type 1 or type 2 diabetes and Sitagliptin also for people with type 2 diabetes. Some diabetes medications help the pancreas release more insulin (if you have type 2 diabetes), others help cells use insulin better, and others keep the liver from releasing too much glucose. The new treatments focus action on hormones called incretins.
Related Conferences: 20th Asia Pacific Diabetes Conference July 16-17, 2018 Sydney, Australia; International Conference on Diabetes and its Complications May 21-22,2018 Osaka, Japan; 25th Global Diabetes Summit and Medicare Expo December 04-05, 2017 Dubai, UAE;23rd International Conference on Herbal and Alternative Remedies for Diabetes and Endocrine Disorders November 2-4, 2017 Bangkok, Thailand; 27th European Diabetes Congress June 11-12, 2018 Rome, Italy; 22nd International Congress on Prevention of Diabetes and Complications October 12-13, 2017 London, UK; 9th Annual Congress on Endocrine Disorders and Therapies October 30- November 1, 2017;
Summary of Diabetes Asia Pacific 2018:
20th Asia Pacific Diabetes Conference is among the World's leading Scientific Conference. The three day event on Diabetes will host 60+ Scientific and technical sessions and sub-sessions on cutting edge research and latest research innovations in the field of Diabetes and Endocrinology and relevant biomedical sciences across the globe. This year annual Diabetes Conference will comprises of 13 major sessions and 104 sub-sessions designed to offer comprehensive sessions that address current issues in Diabetes & Endocrinology, Pancreatic Disorders & Therapy, Steroids & Hormonal Science.
Importance & Scope:
Conference on Diabetes is focusing on various topics, which will target a higher number of audiences. This conference will provide a platform to broadcast the new advancements in the field of diabetes and endocrinology background. Diabetes conference will bring together academic and industrial professions, leading to a brand new experience. We all know it is easier to understand the research from the researcher and more helpful rather than reading it from the journal.
Why Sydney???
The exact number of people with diabetes in Australia is difficult to estimate, but it is likely that more than 1.1 million Australians are living with the disease. Type 2 diabetes accounts for approximately 85 per cent of people with diabetes. Approximately 12 per cent of Australians with diabetes are diagnosed with type 1 diabetes. Around 12 to 14 per cent of pregnant women will develop GDM. Diabetes has a significant, and often preventable, impact on the health and wellbeing of the Australian population. In 2011, diabetes was the underlying cause of 3 per cent of all deaths and an underlying or associated cause of 10 per cent of all deaths. There are a significant number of diabetes-related complications, many of which are preventable. They include heart attack, stroke, amputation, blindness, kidney failure, depression and nerve disease. Prediabetes was examined as part of the Australian Diabetes, Obesity and Lifestyle Study (AusDiab), which found that 16 per cent of adults over the age of 25 years — approximately 2.5 million people — have prediabetes . Between 15 and 30 per cent of people with prediabetes are likely to develop type 2 diabetes within five years. It is difficult to estimate the total economic and social impact of diabetes. Health care that is directly attributable to diabetes costs approximately $1.7 billion per year. In terms of indirect costs, the full cost of diabetes may be as high as $14 billion per year. These indirect costs include reduced productivity, absence from work, early retirement and premature death and bereavement. Costs are heavily concentrated in particular sub-groups of people with diabetes. Annual direct costs for people with diabetes complications are more than twice as much as for people without complications: $9600 compared with $3500.
Approximately 1 million Australians have been diagnosed with diabetes. The prevalence of particularly type 2 diabetes, rises with age and is higher in men than in women. The onset of type 1 diabetes is typically at an early age, thus it is the most common form of childhood diabetes although it can occur at any age. Australia is ranked 7th highest in the world for prevalence of type 1 diabetes in children aged 0-14 years and 6th highest for incidence. Adding to this, there is a growing number of children and adolescents who are now affected by type 2 diabetes.
Diabetes is associated with a myriad of complications which affect the feet, eyes, kidneys, and cardiovascular health. Nerve damage in the lower limbs affects around 13% of Australians with diabetes, diabetic retinopathy occurs in over 15% of Australians with diabetes, and diabetes is now the leading cause of end-stage kidney disease. In people with diabetes, cardiovascular disease (CVD) is the primary cause of death, with around 65% of all CVD deaths in Australia occurring in people with diabetes or pre-diabetes. Furthermore, 41% of people with diabetes also report poor psychological well-being with reports of anxiety, stress, depression and feeling ‘burned-out’ from coping with their diabetes. Moreover, diabetes is ranked in the top 10 leading causes of death in Australia.
Conference Highlights
- Pre-Diabetes/Borderline Diabetes (Pre-cursor to Diabetes Mellitus)
- Influence of genetics on Diabetes
- Metabolic Syndrome / Syndrome X
- Insulin- Important Pancreatic hormone
- Diabetic Kidney Disease (Diabetic Nephropathy)
- Diabetic Eye Disease (Diabetic Retinopathy)
- Complications of Diabetes
- Diabetic Transplantations
- Important Tests to Diagnose Diabetes
- Management of Diabetes
- Diabetes Oral Medications/Anti-Diabetic Medications
- Approaches and technologies for the Treatment of Diabetes
-
New Diabetes Treatments-Enhanced blood flow
Major Diabetes Research Associations around Asia Pacific
- Diabetes Australia Research Program
- Juvenile Diabetes Research Foundation (JDRF)
- The Australian Centre for Behavioural Research in Diabetes
- The Diabetes Research Foundation Western Australia
- The John Curtin School of Medical Research
- The NHMRC Centre of Clinical Research Excellence on Clinical Science in Diabetes (Diabetes CCRE)
- Baker
- The Walter and Eliza Hall Institute of Medical Research
- Diabetes Australia
- Austrian Diabetes Association
- Dietitians Association of Australia
- Diabetes Association Brisbane
- Canadian Diabetes Association in Sydney
Major Diabetes Research Associations around Globe
- International Diabetes Federation
- American Diabetes Association
- Canadian Diabetes Association
- Diabetes New Zealand
- Diabetes United Kingdom
- Glycosmedia
- Diabetes Indian Association
- Diabetes Australia
- Austrian Diabetes Association
- Diabetes UK
- Diabetes South Africa
- Spanish Diabetes Society (Spain)
- Swedish Diabetes Association
- Korean Diabetes Association
Target Audience:
- Endocrinologists
- Diabetologists
- Researchers
- Practitioners/Doctors
- Students
- Nurse educator
- Podiatrist
- Dietitian
- Eye Doctors
- Nephrologists
- Physical trainer or Exercise physiologist
Universities Associated with Cosmetology 2017
Major Universities on Diabetes Research
- Albany Medical College
- Baylor College of Medicine
- Creighton University School of Medicine
- Dartmouth Medical School
- Florida International University College of Medicine
- Georgetown University School of Medicine
- Howard University College of Medicine
- Harvard Medical School
- Johns Hopkins University School of Medicine
-
Pennsylvania State University College of Medicine
Companies Associated with Diabetic products and their funding
Conference Highlights
- Pre-Diabetes/Borderline Diabetes (Pre-cursor to Diabetes Mellitus)
- Metabolic Syndrome / Syndrome X
- Insulin- Important Pancreatic hormone
- Important Tests to Diagnose Diabetes
- Diabetic Kidney Disease (Diabetic Nephropathy)
- Diabetic Eye Disease (Diabetic Retinopathy)
- Diabetic Transplantations
- Diabetes Oral Medications/Anti-Diabetic Medications
- Approaches and technologies for the Treatment of Diabetes
- Complications of Diabetes
- Influence of genetics on Diabetes
- Management of Diabetes
- New Diabetes Treatments-Enhanced blood flow
- Cellular and Molecular Endocrinology
- Endocrine complications
- Endocrine system and metabolic diseases
- Adrenomyeloneuropathy- Rare Genetic Disease
To share your views and research, please click here to register for the Conference.
To Collaborate Scientific Professionals around the World
| Conference Date | July 16-17, 2018 | ||
| Sponsors & Exhibitors |
|
||
| Speaker Opportunity Closed | Day 1 | Day 2 | |
| Poster Opportunity Closed | Click Here to View | ||
Useful Links
Special Issues
All accepted abstracts will be published in respective Our International Journals.
- Journal of Diabetes & Metabolism
- Pancreatic Disorders & Therapy
- Journal of Steroids & Hormonal Science
Abstracts will be provided with Digital Object Identifier by