Day 2 :
Keynote Forum
Gerald J Prudhomme
University of Toronto, Canada
Keynote: Treatment Of Human Pancreatic Beta Cells With A Combination Of Gamma-Aminobutyric Acid (Gaba) And Glp-1 Ameliorates Cell Survival And Proliferation
Time : 10:-00-10:45

Biography:
Gerald J Prud'homme is a Professor in the Department of Laboratory Medicine and Pathobiology at the University of Toronto, and Clinician-Scientist at St. Michael’s Hospital, Toronto. He received his MD degree from the University of Ottawa, Canada (1977) and subsequently specialized in Pathology. He is a Research Fellow at the Institute of Immunology, University of Toronto, the Scripps Research Institute and the McGill Cancer Centre (McGill University, Montreal). Subsequently (1985-2002), he worked as a Scientist and Pathologist in the Department of Pathology, McGill University. His main research interests are in the areas of immunotherapy of autoimmune diseases and cancer therapy.
Abstract:
An effective therapy for type 1 diabetes (T1D) requires the protection of pancreatic beta cells against autoimmunity (immunosuppression and/or anti-inflammatory activity) and beta-cell proliferation or regeneration. No current treatment achieves both goals in a clinical setting. The incretin hormone GLP-1 is effective in the treatment of type 2 diabetes (T2D), but not T1D. Recent studies by us and others have shown that GABA protects beta cells against autoimmune injury and induces their regeneration in mice. In this study, we investigated the effects of these drugs on human islets cells, and compared their response to rodent insulinoma cell lines. We found that GABA increases SIRT1 and Klotho (mRNA and protein), and prevents apoptosis induced by high glucose levels or inflammatory cytokines. Importantly, both Klotho and SIRT1 inhibit the activation of NF-kB. The NF-kB inflammatory pathway provokes beta-cell apoptosis, such that its blockade is protective. We show that a GLP-1 receptor (GLP-1R) agonistic drug ameliorates the effects of GABA in some assays. However, we observed that a GLP-1R agonist does not stimulate human beta-cell proliferation, whereas GABA does promote proliferation. We conclude that GABA, especially when combined with GLP-1, effectively protects human beta islet cells against glucotoxicity and other injuries, and that GABA (but not GLP-1) stimulates their proliferation. These observations suggest that GABA+GLP-1 therapy will be effective in human T1D, due to a combination of anti-apoptotic, anti-inflammatory and proliferative/regenerative effects.
Keynote Forum
Moorkath Nandakumaran
University of Kuwait, Kuwait
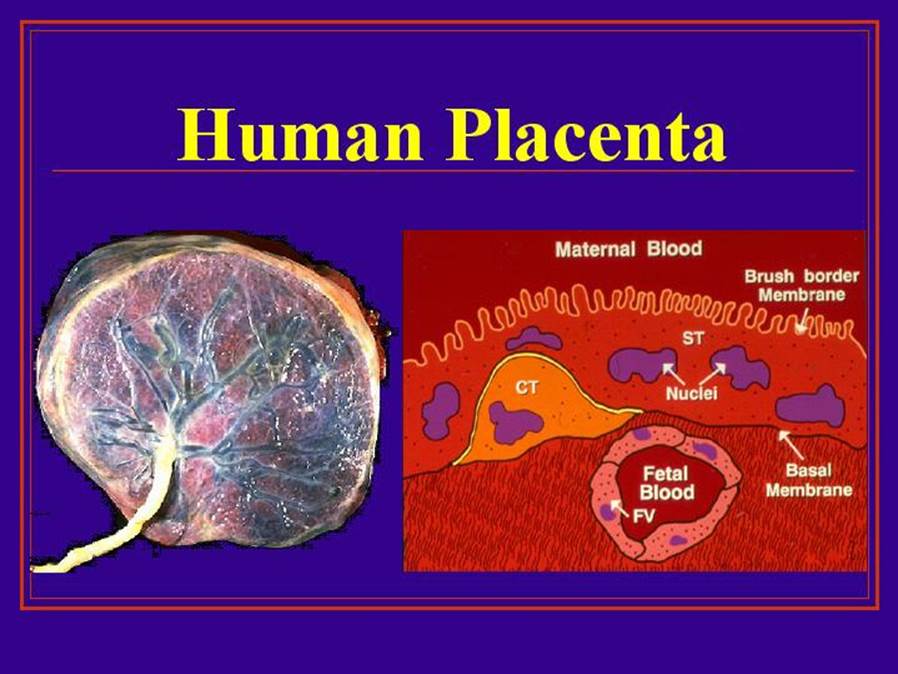
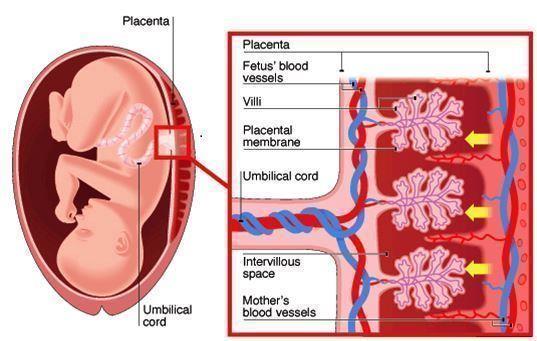
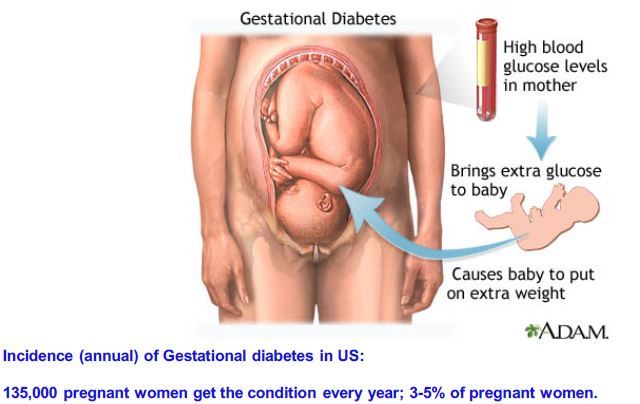
Keynote: Maternal-Fetal Transport Kinetics Of 3-O-Methyl Glucose In Diabetic Model Perfused Human Placenta: In Vitro Study
Time : 10:45-11:30

Biography:
Moorkath Nandakumaran obtained his Doctorate degree in Reproductive Physiology from University of Paris VI in 1979 and has done his specialization in maternal-fetal transport of nutrients and drugs across the human placenta as well as experimentally induced diabetic rats for the past many years. He has been an Invited Speaker for more than six international conferences and has developed human placental perfusion models for study of pregnancy related conditions such as pre-eclampsia and diabetes. He has published nearly 40 papers in international journals related to the area of maternal-fetal transport in health and disease states.
Abstract:
Previous studies from our laboratory had shown that maternal-fetal transport kinetics of model amino acids such as alpha-aminoisobutyric acid and L-Leucine and model fatty acid, palmitic acid were compromised in diabetic model placental lobules perfused in vitro. This study was meant to explore whether transport kinetics of a model hexose, 30-methyl glucose were altered in diabetic model human placental perfusions in in vitro conditions. Human placentae were collected immediately after delivery and perfused with NCTC culture medium buffered with Earles salt solution perfusate. After wash-out period of about ten minutes, 14-C labeled 3-0-methyl glucose (specific activity: 59 mCi/mmol, Amersham, UK) along with tritiated water (specific activity 5 mCi/mmol, Amersham, UK) as reference marker were then injected as a single bolus (100 ml) into the maternal arterial circulation of perfused placental lobules and perfusate samples collected from maternal and fetal circulations over a period of 5 minutes. In another series of experiments, glucose concentration in maternal arterial perfusate was doubled to about 11 mmol/L to mimic a moderate hyperglycemic diabetic state and prefusions were done for five minutes in the control euglycemic series. Concentration of 14C and 3H labeled study and control substances in perfusate samples in control and diabetes model perfusions was assessed by scintillation spectrometry. Transport kinetics of 3-O-methyl glucose and tritiated water were computed using established permeation parameters. Differential transport rates of 3-O-methyl glucose and tritiated water in 8 perfusions differed significantly (Student's t-test; p<0.05) for all transport fractions studied in control perfusions and in perfusions from five diabetic model perfusions. Transport fraction index of 3-O-methyl glucose compared to reference marker averaged 29.9% in control perfusions (n=8) and 33.90% in diabetic model perfusions pregnancies (n=5), respectively. The difference observed in TF index of 3-O-methyl glucose compared to tritiated water in control and diabetic groups were not statistically significant (Student's t-test, p>0.05). Our studies show for the first time that transport behavior of a model hexose, 3-O-methyl glucose is not significantly different or compromised in diabetic model perfusions. We are unable to speculate whether transport kinetics of hexoses could be altered in diabetic pregnant women in vivo state with moderate hyperglycemia as in this study or in diabetic state with greater glucose load than 11 mmol/L as in severe diabetic state.
Keynote Forum
H Henry Dong
University of Pittsburgh, USA
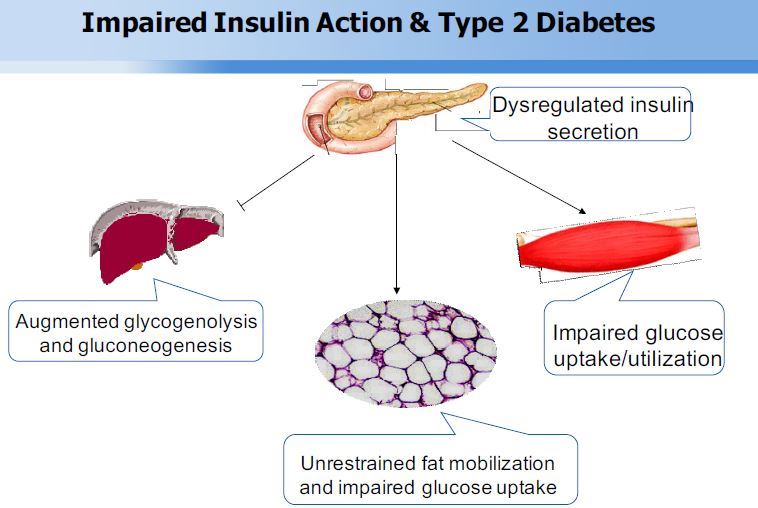
Keynote: Foxo Transcription Factors In Type 2 Diabetes
Time : 11:45-12:30

Biography:
H Henry Dong is the Professor of Pediatrics, University of Pittsburgh School of Medicine, Pittsburgh, USA. He is a member of American Diabetes Association. He is serving as an Editorial Board Member of Journal of Biological Chemistry, Molecular Metabolism, and Journal of Diabetes and its Complications.
Abstract:
The forkhead box O family consists of FoxO1, FoxO3, FoxO4 and FoxO6 proteins in mammals. They share a common structural motif, namely the “forkhead box” or “winged helix” domain that is responsible for binding to chromatin DNA in the nucleus of cells. FoxO proteins act as nuclear transcription factors that mediate the inhibitory action of insulin or insulin-like growth factor on key functions in diverse pathways including cell metabolism, proliferation, differentiation, oxidative stress, cell survival and senescence, autophagy and aging in mammals. Genetic mutations in FoxO genes or abnormal expression of FoxO proteins are associated with metabolic disease, cancer or altered lifespan in humans and animals. My laboratory focuses on the studies of FoxO1 in glucose and lipid metabolism. FoxO1 is abundantly expressed in the liver and its transcriptional activity is tightly regulated by insulin. Insulin inhibits FoxO1 activity via a distinct mechanism by altering its subcellular redistribution. We showed that insulin signaling bifurcates at FoxO1 in the liver to govern two metabolic pathways, namely gluconeogenesis and very low-density lipoprotein (VLDL) assembly. This effect helps synchronize hepatic insulin signaling to simultaneously adjust the rates of hepatic glucose production and VLDL secretion in response to nutrient availability. Such FoxO1-dependent mechanism seems pivotal for the liver to rapidly adapt to metabolic shift between fasting to feeding states for maintaining normal glucose and lipid homeostasis. Our studies provided mechanistic insights into how FoxO1 orchestrates insulin action on hepatic glucose and lipid metabolism in healthy individuals, and how FoxO1 dysregulation, resulting from insulin resistance, contributes to the dual pathogenesis of hyperglycemia and hyperlipidemia in obesity and type 2 diabetes. We screened for small molecule drugs against FoxO1, demonstrating that pharmacological FoxO1 inhibition translated into a significant beneficial effect on glucose and lipid metabolism in mice with diabetic dyslipidemia. Our studies characterize FoxO1 as a potential therapeutic target for improving blood glucose and lipid profiles in type 2 diabetes.
- Treatment of Diabetes | Diabetes Medication & Therapy | Type 2 diabetes & Obesity | Diabetes Melitus|Diabetes Research | Diabetes Chronic Complication
Location: Vasco de Gama 2

Chair
Arturo Solis Herrera
Human Photosynthesis Research Center, Mexico

Co-Chair
H Henry Dong
University of Pittsburgh, USA
Session Introduction
Hidekatsu Yanai
National Center for Global Health and Medicine Kohnodai Hospital, Japan
Title: Possible Vascular And Renal Protective Effects Of Sodium-Glucose Co-Transporter 2 Inhibitors
Time : 12:12-12:45

Biography:
Hidekatsu Yanai is a Fellow of American College of Physicians (FACP), is the Director of the Department of Internal Medicine and Clinical Research and Trial Center, National Center for Global Health and Medicine Kohnodai Hospital, Japan. He obtained his MD and PhD degrees in National Defense Medical College and Hokkaido University School of Medicine, respectively. He was an Invited PhD Research Fellow at the National Institute of Health (NIH), USA. He is the Editor-in-Chief of Journal of Endocrinology and Metabolism and also an Editorial Board Member of ten medical journals. He has 168 published papers in reputed medical journals.
Abstract:
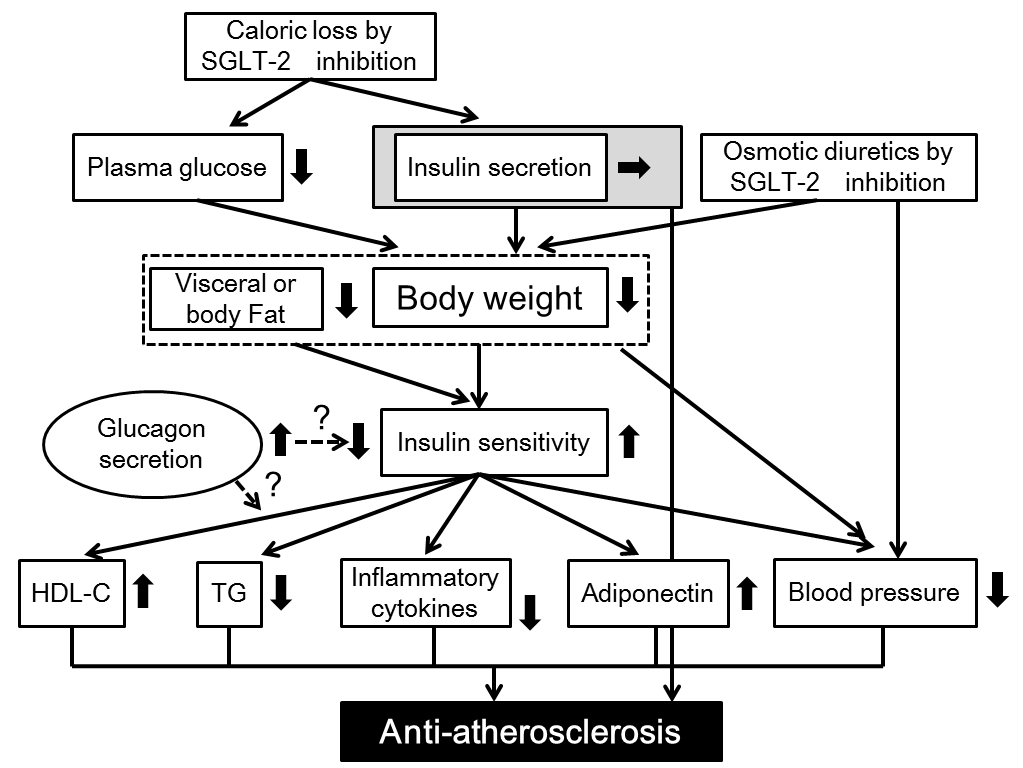
The new drug for type 2 diabetes, the sodium-glucose co-transporter 2 inhibitors (SGLT2i), leads to reduction of renal tubular glucose reabsorption and reduction of plasma glucose, in an insulin-independent manner. For the treatment of diabetes, in addition to glucose control, the management of coronary risk factors is crucial. First, the author searched for the published articles about the possible anti-atherosclerotic effects beyond glucose lowering of SGLT2i, by using PubMed, and found that SGLT2i are proved to be significantly associated with weight loss and reduction of blood pressure by a relatively large number of studies. Second, we retrospectively picked up patients who had been continuously prescribed SGLT2i by a chart-based analysis, and compared the data before the SGLT2i treatment with the data at 1, 2, 3 and 6 months after the SGLT2i treatment started, and found that SGLT2i significantly reduced HbA1c and body weight and improved liver function. Further, the author found a significant difference in hypoglycemic effect between canagliflozin with a low potency to inhibit SGLT1 and tofogliflozin which is a highly selective SGLT2 inhibitor. As the key to resolve this issue, a different distribution between SGLT1 (intestine) and SGLT2 (kidney) came to my mind. SGLT2i with potency to inhibit SGLT1 may be more effective to lower glucose as compared with highly selective SGLT2i, in patients with renal insufficiency. To understand an influence of the estimated glomerular filtration rate (eGFR) on improvement in metabolic parameters by SGLT2i, we sub-analyzed our study and discovered that body weight decreased by SGLT2i, independently of eGFR, however, the changes in HbA1c and liver function depended on eGFR. Recently, Sano reported that elevation of hematocrit by SGLT2i may be a surrogate marker for recovery from reversible tubulointerstitial injury; it was found that erythropoietin could be one of renoprotective effects of SGLT2i.

Guido Lastra
University of Missouri Columbia, USA
Title: Perivascular Adipose Tissue, Inflammation And Insulin Resistance: Link To Vascular Dysfunction And Cardiovascular Disease
Time : 12:45-13:15

Biography:
Guido Lastra is specialist in Internal Medicine and Endocrinology. He is a research-oriented assistant professor at the University of Missouri in Columbia. His area of interest is the pathogenesis of chronic over-nutrition induced insulin resistance and cardiovascular disease. He is focused on studying the role of the mineralocorticoid receptor in the development of insulin resistance-mediated vascular dysfunction. In particular, he is actively exploring the interactions between inflammation and mineralocorticoid receptor activation that lead to vascular stiffness. Dr. Lastra has presented his research in several prestigious International conferences, including the International Aldosterone Conference, the Endocrine Society Meeting, and the American Heart association (High Blood Pressure Council) Meeting. Dr. Lastra has more than 50 publications in peer-reviewed journals, frequently as first author, in prestigious journals including, Diabetes, Endocrinology, Hypertension, and the American Journal of Physiology (AJP). He has served as reviewer for important journals, including Diabetes, Diabetes Care, and the Lancet.
Abstract:
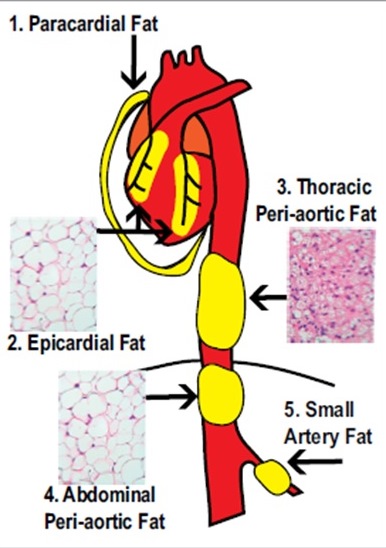
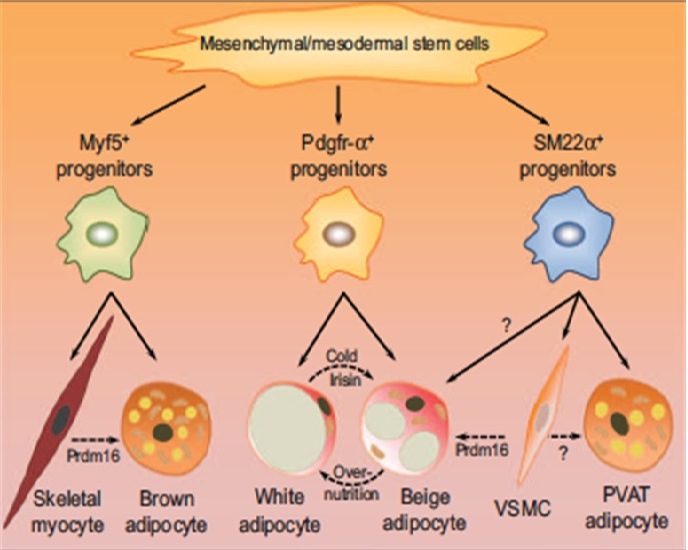
Obesity is a leading risk factor for the development of type 2 diabetes mellitus (DM2) and cardiovascular disease (CVD), however the underlying mechanisms still remain to be fully uncovered. It is now well accepted that dysfunctional adipose tissue in conditions of obesity is a critical source of inflammation that impacts the cardiovascular system and contributes to CVD. Although traditionally visceral adipose tissue has been linked to increased CVD risk, there is mounting interest in the role that fat accumulation around the vasculature plays in the pathogenesis of vascular dysfunction. Perivascular adipose tissue – PVAT- is in intimate contact with large, medium and small diameter arterial beds in several tissues, and has been shown to control vascular function as well as remodeling. PVAT does not merely mirror visceral adipose tissue changes seen in obesity, but has unique features that impact vascular biology. In lean individuals PVAT exerts vasodilatory and anti-inflammatory functions, however obesity results in PVAT inflammation, characterized by imbalance between pro and anti- inflammatory cells as wells as adipokines. PVAT inflammation promotes insulin resistance in the vasculature, thus resulting in impaired insulin-mediated vasodilatory responses and vascular remodeling. In this review we address current knowledge about the mechanisms that link PVAT inflammation to insulin resistance and vascular dysfunction. Indeed, PVAT emerges as a novel type of adipose tissue that participates in the pathogenesis of CVD, independently to a large extent to visceral adipose tissue.
Irina Kurnikova
RUDN University, Russia
Title: The Phenomenon Of Early Aging Of Regulatory System In Diabetes Type 2
Time : 14:00-14:30

Biography:
Irina Kurnikova is a Professor of Medicine, RUDN University (Peoples Friendship University of Russia), Russia. She has done her PhD in 2010. She has dealt with the problems of endocrinology for more than 20 years. She had led a course of Endocrinology at the Medical Academy (Izhevsk, Russia), Endocrinology department of Russian Scientific Center of Medical Rehabilitation and Health Resort, Russia. Currently, she teaches at Peoples' Friendship University of Russia, Curator of the Scientific Direction of Endocrinology. She has published more than 20 articles in well-known journals, and is the author of 25 books and manuals in Russian.
Abstract:
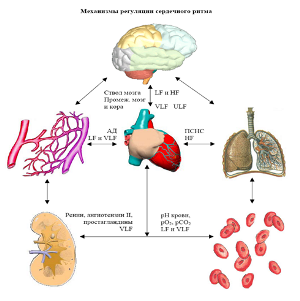
Statement of the Problem: Three systems provide the physiological functioning and interaction with the environment: Autonomic nervous regulation, endocrine-metabolic system and immune system. The most operational system of autonomic regulation, the level of functioning of which varies with age and systemic disorders inside the body. The purpose of this study is to assess the impact of diabetes mellitus on mechanisms of autonomic regulatory in different age groups.
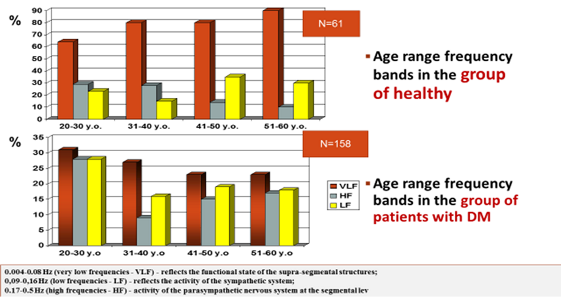
Methodology & Theoretical Orientation: 101 people were divided in four age groups: 20-30 years, 31-40 years, 41-50 years and 51-60 years of age. All patients were evaluated based on autonomic regulation by the method of spectral analysis of daily variability of the heart rhythm power spectrum of oscillation in three frequency bands: 0.004-0.08 Hz (very low frequency – VLF), 0.09-0.16 Hz (low frequency – LF) and 0.17-0.5 Hz (high frequency – HF). The selection of three frequency ranges is due to differences in their formation. The low frequency range reflects the activity of the sympathetic system on the segmental level, the high-frequency range, the activity of parasympathetic nervous system at the segmental level.
Findings: Patients with diabetes at the age of 30-40 years we have seen a decrease in parasympathetic activity, which is more typical for patients the next decade of life. Since the age of 41, there was considerable centralization on mechanism of regulation (increase VLF), which usually starts 10-15 years later. The decrease in the total power spectrum on the background of inadequate compensator of diabetes showed decrease of reserve opportunities of the organism.
Conclusion & Significance: An important cause of early atherosclerosis in patients with diabetes is, in addition to endothelial dysfunction, syndrome of “early aging of regulatory system” (the reason - autonomic neuropathy). The status autonomic regulation in the current decade corresponds next age decade of the patient, which leads to increased comorbidities and increased cardiovascular risk.
Bandar Manawer Al Harbi
Prince Sultan Military Medical City, UK
Title: The Impact Of A Combined Aerobic And Resistance Exercise Programme In Preventing Or Delay To The Onset Of Diabetes For Subjects At Risk
Time : 14:30-15:00
Biography:
Bandar Manawer Al Harbi, Assistant Director of Pharmacy for Material Management, Prince Sultan Military Medical City, (PSMMC).
Abstract:
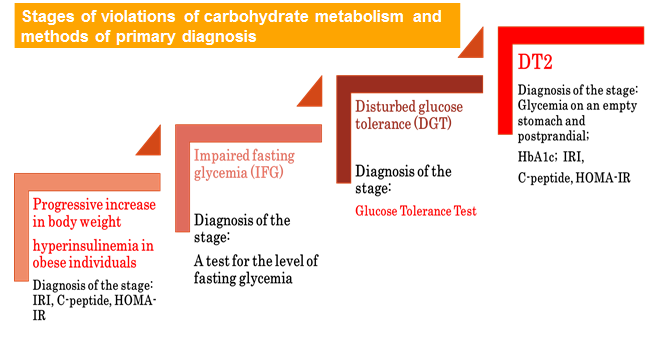
Prediabetes describes a condition whereby an individual’s level of blood glucose is above normal level, though not high enough to warrant them a T2D diagnosis. The condition is classified into two categories; impaired glucose tolerance (IGT) where blood glucose levels are above the normal 2 hours after glucose loading in the oral glucose tolerance test but not so high to warrant the classification as diabetes. The other is impaired fasting glucose (IFG) where blood glucose have risen to a fasting state but yet again, not so high to warrant the classification as diabetes. Physical exercise improves BG homeostasis but the extent to which exercise is effective strategy as primary prevention mechanism for people whom at risk to develop diabetes is not fully understood.
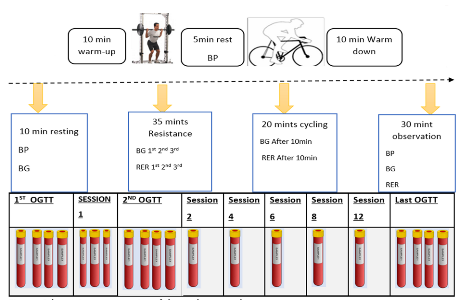
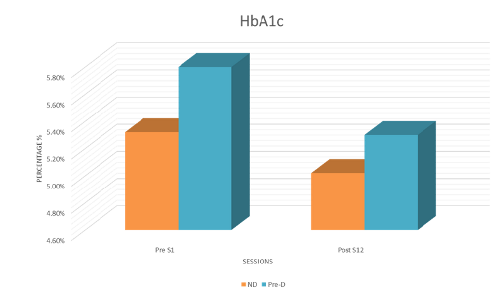
Purpose: To examine the effects of 6-weekes moderate-intensity combined aerobic and resistance exercise program in preventing or delaying the onset of diabetes for subjects at risk compared to sedentary non-diabetic individuals. Methods: 20 subjects of a sedentary lifestyle, diagnosed with either prediabetes or at risk to developed T2D (PRE-D) and 5 Subjects were sedentary healthy individuals (ND) met the inclusion criteria. Both PRE-D and ND have been asked to complete 6-weeks of moderate-intensity combined aerobic and resistance exercise for 60 minutes on two days/week. Each exercise session consists of a combined exercise protocol of 30 minutes of resistance exercise (3 sets of 10 repetitions) followed by 20 min cycling. The primary outcome is to concentrate on metabolic results, such as improved HbA1c, blood pressure, heart rate, 1-repition max, lipid profile (reduction in Total Cholesterol, Low Density Lipoproteins, Triglycerides or increase High Density Lipoproteins) and improvements in insulin sensitivity determined by responses to oral glucose tolerance tests on independent days.
Mehdi Khalfallah
Charles Nicolle’s Hospital, Tunisia
Title: Which germs should be targeted in diabetic foot infection? A prospective study of 100 patients
Time : 15:00-15:30

Biography:
Mehdi Khalfallah has completed his Medical studies from Faculty of Medicine of Tunis, Tunisia. He is an Assistant Professor in Surgery at Charles Nicolle’s Hospital since 2012. He is an Editorial Board Member and Drafting Committee Member of “la Tunisie Médicale” (indexed in PubMed, impact factor=0.3). He has published more than 15 papers in reputed journals.
Abstract:
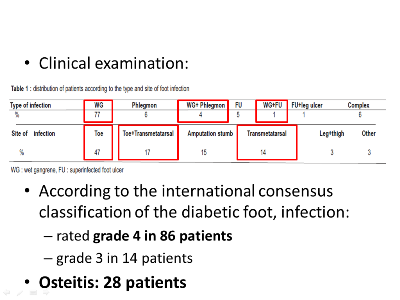
Background & Aim: Identifying the infecting bacterial flora is one of the main rules to be followed to ensure the success of antibiotherapy in the treatment of the infected diabetic foot. The aim of the work was to define the bacteriological profile of the bacteria causing the infection of the diabetic foot at the Surgery Unit B of Charles Nicolle’s Hospital in Tunis and determine the prognostic factors of this condition.
Methods: It was an open prospective study. It concerned 100 diabetic patients operated on for diabetic foot infection. All patients had bacteriological samples taken through deep scraping and swabbing carried out in the operating room.
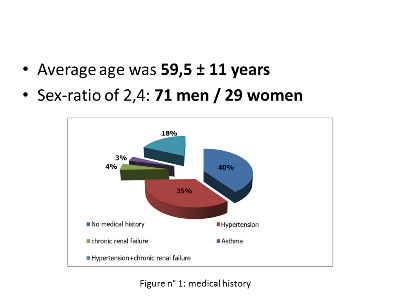
Results: The average age of patients was 59.5±11 years, with a sex ratio of 2:4. The foot infection was represented in 82% of cases by a wet gangrene. The enterobacteria were the most frequently isolated bacteria (73%), followed by Streptococcus (10%), Staphylococcus aureus (9%). The rate of multidrug-resistant bacteria was of 9.5%. The empiric antibiotic therapy used (fusidic acid+amoxicillin/clavulanic acid) was inactive on 44.1% of the isolated bacteria. When we compared the group of patients with unfavorable development (who have been re-operated) and the group of patients with favorable development, we have found two poor prognosis factors: arteritis (p=0.018; OR=23.7) and presence of multidrug-resistant bacteria (p=0.027; OR=5.8).
Conclusion: The enterobacteria were the main bacteria causing the infection of diabetic foot. The prognostic factors found, arteritis and isolation of multidrug-resistant bacteria; outpoint the importance of multidisciplinary care.
Mehdi Khalfallah
Charles Nicolle’s Hospital, Tunisia
Title: Predictive Factors For Major Amputation Of Lower Limb In Diabetic Foot Of About 430 Patients
Time : 15:45-16:15

Biography:
Mehdi Khalfallah has completed his Medical studies from Faculty of Medicine of Tunis, Tunisia. He is an Assistant Professor in Surgery at Charles Nicolle’s Hospital since 2012. He is an Editorial Board Member and Drafting Committee Member of “la Tunisie Médicale” (indexed in PubMed, impact factor=0.3). He has published more than 15 papers in reputed journals.
Abstract:
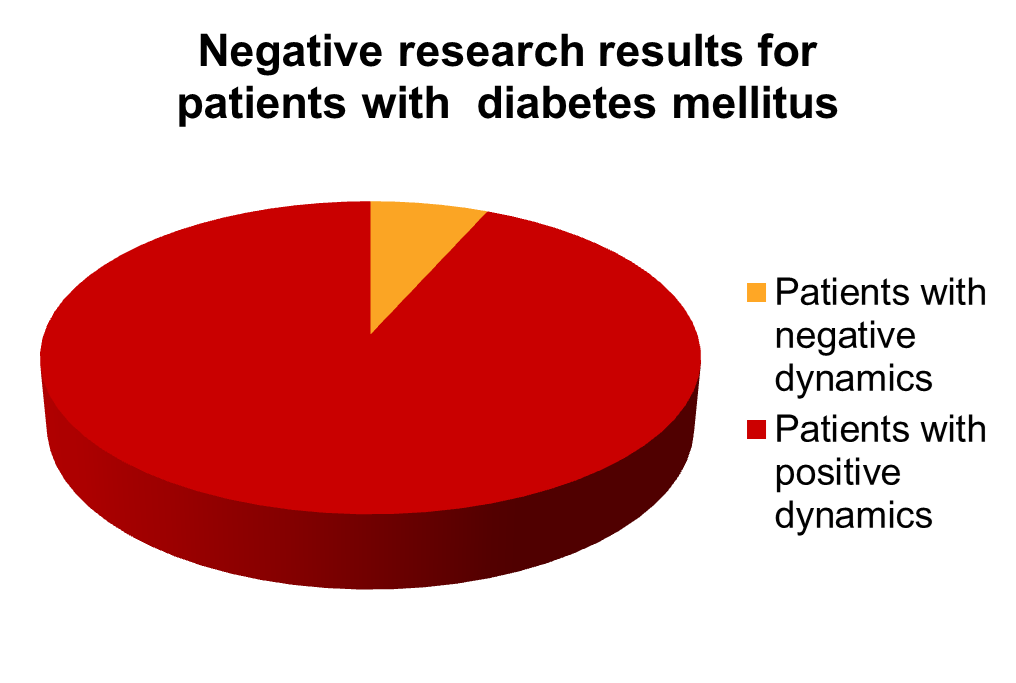
Background & Aim: Major amputation of the lower limb is defined by a leg or thigh amputation. The aim of our work was identifying predictive factors for lower limb major amputation in patients with diabetes admitted on for foot lesions through using an administrative data base.
Methods: It was a retrospective study ranging from June 1st, 2008 to December 31st, 2011, which included all the patients admitted on for an infected diabetic foot to the Surgery Unit B of Charles Nicolle Hospital in Tunis. The main judgment criterion was the major amputation of the lower limb. We have done a descriptive and a comparative study, with univariate and multivariate analysis.
Results: We have enrolled 319 men and 111 women. The average age was 60.5±12 years. Ninety five patients had a major amputation that is 24% of cases. Former inpatient, patient readmitted within one month post-operatively, stay in intensive care, admission in intensive care within 48 hours after admission, age ≥65 years, presence of kidney problem, preoperative stay and length of intervention were identified as predictive factors of major amputation in the univariate analysis. Age is the only independent variable predictive for major amputation which appeared from the multivariate analysis (p=0,004). The age cut-off ≥65 years have a specificity of 69% and a sensitivity of 47% (p=0.004, OR=1.971, IC 95%: 1.239-3.132).
Conclusions: Age is the only independent predictive factor for major amputation of the lower limb in the diabetic foot with a threshold value higher or equal to 65 years. Patients aged more than 65 had 1.9 times more risk to undergo major amputation of the lower limb.
David Karasek
University Hospital Olomouc, Czech Republic
Title: Selected Adipokines In Patients With Type 2 Diabetes: Relationship To Markers Of Endothelial Dysfunction And Arterial Stiffness
Time : 16:15-16:45
Biography:
David Karásek is an associate professor of Internal Medicine at Faculty of Medicine and Dentistry of Palacky University in Olomouc, Czech Republic. He works as Deputy Head of Third Department of Internal Medicine – Nephrology, Rheumatology and Endocrinology of University Hospital Olomouc. He manages the Center for diabetes of University Hospital Olomouc and as specialist doctor is involved in the activities of the Clinic for endocrine diseases and the Center for lipid metabolism disorders. His research is focused on the issue of dyslipidemia, metabolic syndrome, insulin resistance, visceral obesity and their relationship to early cardiovascular involvement. He is the author or co-author of several chapters in monographs or textbooks and of about one hundred scientific papers. He is the editorial board member for the two scientific journals. For his research, he received a number of medical awards (Prizes of the Czech Society for Internal Medicine, Czech Society for Atherosclerosis, Czech Diabetes Society) and the Minister of Health of the Czech Republic Prize for research and development.
Abstract:
Introduction: Adiponectin, adipocyte fatty acid-binding protein (A-FABP), fibroblast growth factor 21 (FGF-21), C1q/TNF-related protein 9 (CTRP9) and allograft inflammatory factor-1 (AIF-1) differently contribute to oxidative stress, chronic inflammation, insulin resistance and vascular damage. The aim was to compare their levels in patients with type 2 diabetes and in healthy controls and to determine their relationship to markers of endothelial dysfunction and arterial stiffness.
Methods: 54 patients with type 2 diabetes (32 men, 22 women) and 21 healthy controls (8 men, 13 women) were included in the study. Adipokines, lipids, anthropological parameters, indicators of insulin resistance and also soluble markers of endothelial dysfunction - von Willebrand factor (vWF), plasminogen activator inhibitor-1 (PAI-1) and tissue plasminogen activator (t-PA) were measured. Augmentation index (AI) and pulse wave velocity PVW measured by SphygmoCor served as markers of arterial stiffness.
Results: Type 2 diabetics had significantly higher levels of A-FABP [50.0 (38.1-68.6) versus 28.6 (23.6-32.9) mg/l, p<0.001], vWF [133.1 (110.7-163.2) versus 98.5 (84.4-125.0)%, p<0.01] and PAI [78.1 (41.2-106.5) versus 36.9 (27.5-41.9) ng/ml, p<0.001] and lower levels of adiponectin [5.9 (4.3-9.0) versus 11.3 (8.7-14.8) mg/l, p<0.001] compared to healthy controls. Differences in other adipokines were not statistically significant. Adiponectin correlated negatively with vWF levels (r=-0.29, p<0.05) and PAI-1 (r=-0.35, p<0.01), A-FABP positively with vWF (r=0.45, p<0.01) PAI-1 (r=0.46, p<0.01) and augmentation index (r=0.39, p<0.01). The levels of FGF-21 correlated only with PAI-1 (r=0.27, p<0.05).
Conclusion: Patients with type 2 diabetes have significantly higher levels of A-FABP and lower levels of adiponectin. These adipokines correlate with markers of vascular damage and may interfere with the cardiovascular risk of these individuals.
- Treatment of Diabetes | Diabetes Medication & Therapy | Type 2 diabetes & Obesity | Diabetes Melitus | Diabetes Research | Diabetes Chronic Complication
Location: Vasco de Gama 2

Chair
Moorkath Nandakumaran
University of Kuwait, Kuwait

Co-Chair
H Henry Dong
University of Pittsburgh, USA
Session Introduction
Irina Kurnikova
RUDN University, Russia
Title: Serotonin Level And Nutritional Behavior Of Patients With Primary Insulin Resistance
Time : 12:30-13:00

Biography:
Kurnikova Irina is a Professor of Medicine, RUDN University (Peoples Friendship University of Russia), Russia. She has done her PhD in 2010. She has dealt with the problems of endocrinology for more than 20 years. She had led a course of Endocrinology at the Medical Academy (Izhevsk, Russia), Endocrinology department of Russian Scientific Center of Medical Rehabilitation and Health Resort, Russia. Currently, she teaches at Peoples' Friendship University of Russia, Curator of the Scientific Direction of Endocrinology. She has published more than 20 articles in well-known journals, and is the author of 25 books and manuals in Russian.
Abstract:
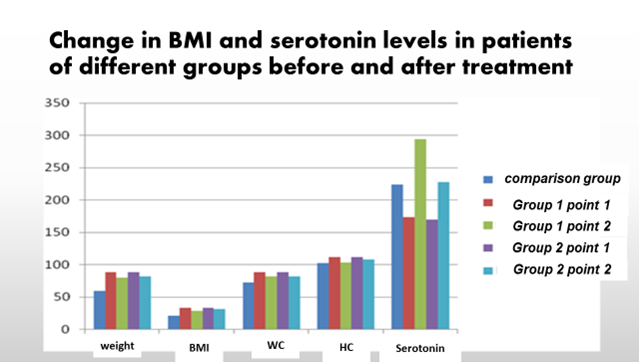
Statement of Problem: One of the most important tasks at the initial stage of treatment of patients with primary insulin resistance is a weight loss, which means a decrease in the amount of food consumed. Patients rarely manage to cope with this task independently, and drug therapy does not always provide sufficient effect.
Purpose of Study: To evaluate the effect of acupuncture on the production of serotonin and especially eating disorders patients with primary insulin resistance.
Methods & Theoretical Orientation: Patients (42 people) aged 38.4±2.0 years, body mass index (BMI) 32.3±4.2 kg/m2 were selected for this study. Two groups of observation were formed: group 1 (20 people) received reflex therapy using special corporal and auricular points and a low caloric diet. Patients of the 2nd group (22 people) were prescribed only a diet. The comparison group consisted of 12 practically healthy persons. We studied: BMI, ratio of OT/OB (waist circumference/hip circumference), HOMA-IR index, insulin and C-peptide. Serotonin in serum was determined by ELISA. Reflex therapy procedures included daily corporal and auricular acupuncture, surface acupuncture according to a certain scheme (11 II, 36III, 7V, 41XI, 60VII, 34, 25, 22, 18 and 55).
Results: A lower serotonin level in the serum of patients in the observation groups was noted -173.3±60.8 ng/ml (in the comparison group -223.9±90.4 ng/ml). The relationship between BMI and serotonin concentration in serum r=-0.23 (p=0.04) was revealed. In group 1 there was an increase in serotonin level by 69.5% (p=0.0057), body weight decreased by 9.8%. In group 2 serotonin level increased by 34.4% (p=0.031), and body weight decreased by 7.4% (p=0.051). Patients of group 1 after the course of treatment noted a decrease in appetite, which allows observing the diet and reducing the amount of food.
Conclusion: The use of reflex therapy with the use of special corporal and auricular points promotes serotonin increase in serum and leads to rapid satiety during eating. This allows patients to follow a low caloric diet at the initial stage of treatment.
Abeuova Gulnara
Almaty Institute of Advanced Medical, Kazakhstan
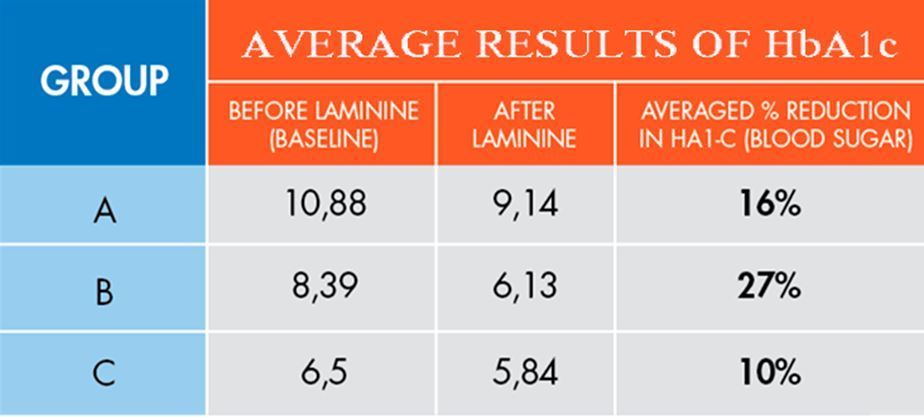
Title: High-Normal Blood Sugar Levels Were Significantly Reduced In Ten Subjects Consuming A High Protein, Active Dietary Supplement For 12 Weeks
Time : 14:00-14:30

Biography:
Abeuova Gulnara. Entered Almaty State Medical Institute in 1976, graduated in 1982. Since 1982 work as a doctor and teach at Medical University as well as at medical college. Specialist - family doctor, doctor of the highest category. I wrote educational materials for students. Personal growth - I took international courses of personal growth with USAID (United States). Specialties: gynecology, oncology, family medicine - in the Almaty Institute of Advanced Medical. Since 2005 I opened up my own medical center “ACAP”. -Director 2005-current.
Abstract:
Metabolic syndrome is primarily a condition of middle aged populations but becoming more prevalent in younger populations. Its criteria are overweight, sedentary lifestyle, and “modern diets” of unhealthy foods. Diet and physical activity are the most modifiable behaviors. The metabolic syndrome is an entity, made up of a cluster of cardiovascular risk factors, which increases risk of future coronary type II diabetes, heart disease, and stroke. The prevalence runs about 20% in most westernized cultures. “Normal” blood sugar, as measured by HbA1-C, has a range of high-, medium- and low-normal ranges to indicate rising blood sugar. When the HbA1-C marker shows values in the high-normal range it indicates the subject is beginning to show abnormal blood sugar and/or insulin resistance. This early detection provides an interim whereby the individual may reverse the pattern. A clinical trial was conducted by the primary physician selecting ten subjects with high normal HbA1-C levels who were not taking medications to manage blood sugar. Subjects were informed about the dietary supplement Laminine (LifePharm Inc., Lake Forest, CA) which contains proprietary fertilized chicken egg extract, shark cartilage and pea protein powders. Subjects signed informed voluntary consent. Subjects were asked to refrain from taking other supplements and maintain routine dietary and exercise patterns. Subjects were instructed to consume two supplements in the morning and two in the evening daily for 12 weeks. A t-test for related samples was performed comparing baseline and 12 week final HbA1-C values showing a statistically significant decrease with a p value of 0.013. Results indicated four Laminine supplements consumed daily for 12 weeks supported lowering high-normal blood sugar values in this study. No untoward side effects were observed. Support for reducing high normal blood sugar with a safe, active dietary supplement warrants further investigations.
Joyce Espinosa
Al Sheehaniya Health Center, Qatar
Title: Psychosocial Aspects Of Living With Diabetes Mellitus: Basis For An Enhanced Diabetic Program Of Primary Health Care In Doha, Qatar
Time : 14:30-15:00

Biography:
Joyce Espinosa is working a Staff Nurse, Al Sheehaniya Health Center, Doha, Qatar
Abstract:
This descriptive-relational study was conducted to determine the psychological and social aspects of living with diabetes mellitus. The findings would be the basis for an enhancement of the diabetic program in primary health care. Using the one-shot survey design, 280 patients with diabetes mellitus were included as respondents of the study. The statistical tools employed were means and frequency distribution for descriptive analysis, while Gamma and Cramer’s V were used for inferential analysis. This research has shown that the respondents were fairly psychologically and socially well. They were satisfied with self and living in a purposeful manner, however, they were anxious about the complications of the disease. Family members were concerned about their condition wherein they could talk freely about diabetes mellitus. Educational attainment and living arrangement were significantly correlated with psychological well-being. Presence of illnesses not related to diabetes was significantly correlated with both psychological and social well-being. In conclusion, patients with diabetes mellitus still have the ability to feel good about themselves, having healthy relationships, and maintain psychological health and social well-being.
Charlotte Clark
Team Consulting Ltd, UK
Title: Technological vs. Emotional needs: what is it really like to have type 1 diabetes? Using design research to guide product innovation
Time : 15:00-15:30

Biography:
Charlotte Clark is a Senior Consultant at Team Consulting; a medical device product development consultancy based in Cambridge, UK. Her work involves managing the strategic and creative ‘front-end’ of the product development process. She utilizes her design research, facilitation skills and knowledge of innovation techniques to understand the needs of the market and determine strategic direction and guide innovation activities - A critical part of the development process resulting in the creation of innovative but realistic solutions. She has 20 years of experience working on medical devices. She has a degree in Medical Engineering, BEng from Cardiff University, and MSc degree from Kings College London.
Abstract:
Diabetes management technology has advanced immensely in recent years, greatly improving the lives of people with type 1 diabetes (T1D). But has this been at the expense of the psychological impact of the disease? Is this expensive technology out of financial reach for many, and is it actually making them think more about their condition when all they want to do is forget about it? As medical device designers, we take a holistic view of the problems we are trying to solve. Not only do we seek to understand issues with current devices, but we also seek to really understand all the practical and emotional challenges of managing a life-long condition. A consideration of this bigger picture could lead to innovations which could make a real difference to people’s lives. We approached 10 active T1D bloggers to take part in a small piece of online design research aimed at uncovering the practical and emotional challenges currently facing people with T1D. Each participant received a short questionnaire and a pack of sugar (a clay modeling material) and was asked to create a model that expressed what it felt like to have T1D. They were also asked to take photos of anything important to them when managing their condition. We did not ask specific questions about the devices they were using, but instead set out to discover more about what it is like living with T1D. This research identified a number of challenges around the 24/7 physical and emotional burden of the disease from the practicalities of managing large amounts of equipment; to the fear of night time hypos; managing diet and exercise; reimbursement; concerns around stigma and simply going out with friends. This talk will present insights into life with T1D and give examples of how these insights could lead to conceptual solutions.
Nurten Terkes
Akdeniz University, Turkey
Title: Psychometric Evaluation Of The Diabetes Distress Scale In Patients With Type 2 Diabetes In Turkey
Time : 15:45-16:15

Biography:
Nurten Terkes completed her Master’s degree in 2012 and doing her PhD at Akdeniz University Institute of Health Sciences. She has many articles published in national and international journals about diabetes mellitus. She participated in many national and international congresses about diabetes mellitus. She is a Research Assistant at Akdeniz University Faculty of Nursing.
Abstract:
Aim: To evaluate the psychometric properties of the Diabetes Distress Scale, as measures of diabetes-related psychosocial symptoms, in patients with type 2 diabetes in Turkey.
Methods: This research was carried out on 170 patients diagnosed with type 2 diabetes in the Department of Endocrinology and Metabolic Diseases of a university hospital in Turkey from 15th September 2016 till 15th January 2017. Personal information forms developed by the researchers and the Diabetes Distress Scale were used as the data tools. The informed consent was obtained from the patients. Descriptive statistics, parametric and nonparametric tests and exploratory factor analysis were used in data analysis.
Results: According to the results of the research, the patients had a mean±standard deviation age 55.9±7.54 years (range, 20–65) and included most patients who were female (64.1%), married (87.1%), housewives (50.3%), and had completed primary education (47.4%). Cronbach’s alpha found reliability for the total scale to be 0.91 and subscale alpha coefficients ranged 0.76–0.85. Exploratory factor analysis resulted in a three factor structure: (1) emotional and regimen distress (9 items), (2) health professional-related distress (4 items), and (3) diabetes-related interpersonal distress (3 items).
Conclusion: The Turkish version of the Diabetes Distress Scale was found to be a reliable and valid means to measure diabetes-related psychosocial symptoms in patients with type 2 diabetes.
Sherry Elisha Mata
Cairo University, Egypt
Title: The Correlation Between Serum Omentin-1 Levels And Insulin Resistance In Type 2 Diabetic Women
Time : 16:15-16:45

Biography:
Sherry Elisha Mata has completed her Master’s degree from Cairo University, Egypt. Currently, she is doing her PhD at the Cairo University, Egypt and Post-graduate Diploma in Diabetes from Cardiff University, England.
Abstract:
Adipose tissue has been known as a source of a variety of bioactive peptides called adipokines. Recently, a new protein omentin-1 (also named intelectin-1, endothelial lectin and intestinal lactoferrin receptor) has been identified as a major visceral (omental) fat secretory adipokine. Omentin is highly and selectively expressed in visceral adipose tissue relative to subcutaneous adipose tissue and together with visceral obesity play important roles in carbohydrate and lipid metabolism, homeostasis, insulin resistance, diabetes and cardiovascular function. Insulin resistance links nutrition, glucose, insulin and adipokines in various metabolic important tissues. While, omentin is highly expressed in human visceral fat tissue, circulating omentin levels are reduced in obese subjects. Omentin is also down-regulated in association with obesity- linked metabolic disorders including insulin resistance, glucose intolerance and type 2 diabetes. The aim from our study was to increase our knowledge about omentin-1 and its relationship with type 2 diabetes mellitus, insulin resistance and obesity. The study included 60 female patients with type 2 diabetes mellitus with their age group (40-60). 30 aged matched female subjects formed the control group. All subjects were subjected to full clinical examination, body weight, height, BMI, waist and hip circumference, fasting plasma glucose, fasting insulin, fasting serum lipid profile, HbA1c and fasting omentin-1 levels. Insulin resistance was calculated as HOMA-IR. We found the serum Omentin-1 significantly lower in cases as compared to control group (p value<0.001). We also found that plasma omentin-1 is inversely related to obesity (negatively correlated to BMI, weight, waist and hip circumference). A statistically significant positive correlation between weight, BMI, waist, hip circumference, fasting glucose, HbA1c, insulin and insulin resistance within cases were detected in our study. In our study, the ROC curve analysis showed that the cutoff value of serum omentin-1 levels was 22.2 pg/mL (yielding sensitivity and specificity values of 100% for both). These results emphasize the usefulness of the discriminant ability of plasma omentin -1 to differentiate between cases (who were obese and having high insulin resistance) and controls. Our study showed that omentin-1 levels are low in type 2 diabetic and insulin resistant females. We also found that plasma omentin-1 is inversely related to obesity (BMI, weight, waist and hip circumference).









